CRISPR gene editing therapies took a big step toward commercialization in the United States last week, as the FDA laid out decision deadlines for the potential approval of exa-cel, developed in partnership between Vertex Pharmaceuticals and CRISPR Therapeutics. Across several years of human trials, exa-cel has been shown to be remarkably safe and effective in treating both sickle cell disease and transfusion-dependent beta thalassemia.
A landmark approval for a CRISPR-based therapy in the US, which could come before the end of the year, has the potential to open the floodgates for one of the most innovative gene editing systems available to biotechnology firms today. If made available commercially, exa-cel is expected to drive billions of Dollars in peak sales.
Related ETF and Stocks: ARK Genomic Revolution ETF (ARKG), CRISPR Therapeutics AG (CRSP), Vertex Pharmaceuticals Incorporated (VRTX), Editas Medicine, Inc. (EDIT)
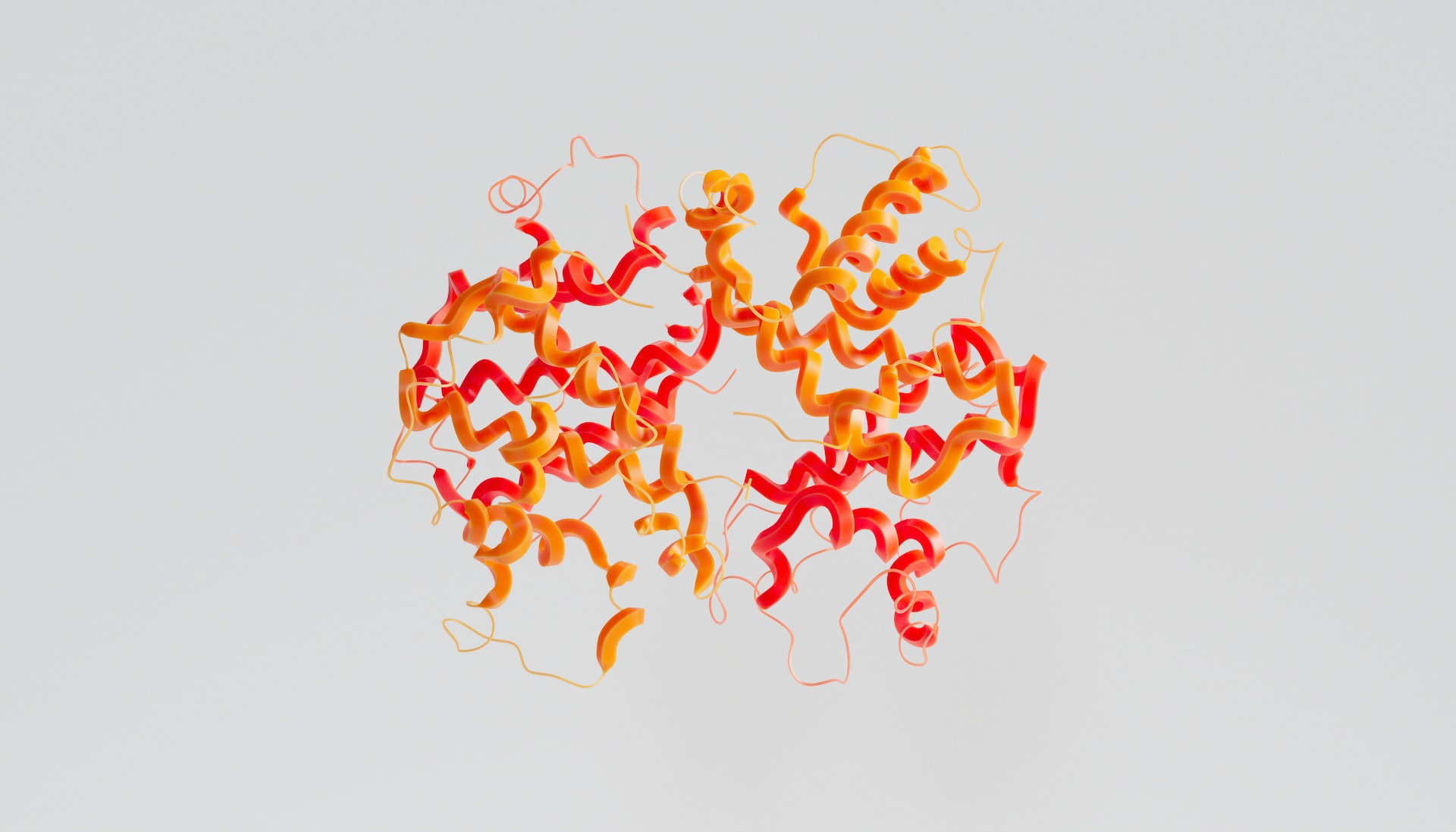
Last week, the US Food and Drug Administration (FDA) agreed to review a candidate therapy that relies on clustered regularly interspaced short palindromic repeats (CRISPR) gene editing technology for the first time. Vertex Pharmaceuticals’ and CRISPR Therapeutics’ exagamglogene autotemcel (exa-cel) received priority review status for its treatment of sickle cell disease (SCD) patients and, therefore, will receive an approval decision by December 8 of this year. A standard review was granted for patients with transfusion-dependent beta thalassemia (TDT) will be concluded by March 30, 2024. New clinical trial data that was released shortly after the FDA announced review periods for potential recipients of exa-cel will add to a mountain of positive results that the breakout gene therapy has banked over the past four years.
MRP has followed exa-cel’s development for some time, even prior to it becoming the very first CRISPR-based treatment to be used in US human trials in 2019. Originally dubbed CTX001, exa-cel was developed by CRISPR and Vertex as part of a $900 million agreement and is a one-time treatment that genetically alters the patient’s own cells to produce the kind of hemoglobin found at birth, which isn’t distorted, allowing red blood cells to work properly. As we highlighted last year, the treatment for SCD and TDT had been 100% effective in clinical studies to that point.
MRP initially covered the trials in 2020 when a trio of patients, two with TDT and one with severe SCD, saw benefits from one-time treatment with the experimental CTX001. After a follow-up of five to 15 months, all three patients were…
To read the complete Intelligence Briefing, current All-Access clients, SIGN IN All-Access clients receive the full-spectrum of MRP’s research, including daily investment insights and unlimited use of our online research archive. For a free trial of MRP’s All-Access membership, or to save 50% on your first year by signing up now, CLICK HERE